Protect Your Liver
You care for it before it surprises you
On this world liver day, the 19th of April 2021, we take the opportunity to explain the importance of the Liver and how vital it is for our body to function optimally.
We all have a fairly good idea about the importance of the heart, kidneys, brain and eyes. This is because these organs and diseases related to these organs are common and most talked about. Three main diseases commonly affecting the heart, kidneys, brain and eyes are diabetes, hypertension and dyslipidemia. These three diseases together comprise the” Metabolic Syndrome”.
Little did we realize that the Liver is the organ that has a significant role in the pathogenesis of the “Metabolic Syndrome”. The Liver is a metabolic workhorse that performs a diverse array of biochemical functions necessary for whole-body metabolic homeostasis. This says that the Liver needs to keep healthy and function optimally, and anything altering the Liver’s function will lead to alteration in the whole-body metabolic homeostasis.
Taking it forward, let us get a brief idea about the problems associated with the Liver. To enumerate a few, we can classify them as:
1. Inherited diseases like Hemochromatosis, Wilsons disease.
2. Infectoins by Viruses like hepatitis A, hepatitis B, and hepatitis C
3. Life style diseases like NAFLD and AFLD are caused by alcohol, foods, obesity diabetes, starting from fatty Liver to cirrhosis to liver failure.
Liver cancer.
NAFLD
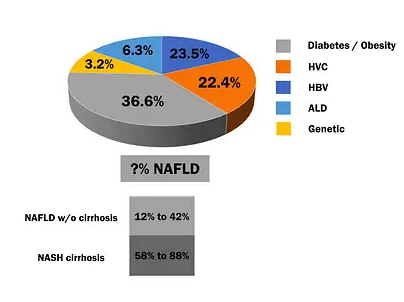
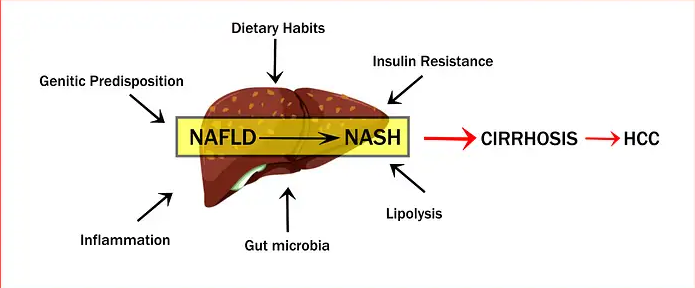
NAFLD includes Fatty Liver (steatosis), NASH (nonalcoholic steatohepatitis )and cirrhosis.
The prevalence rate of NAFLD increases with increasing body mass index (BMI).
The prevalence of NAFLD in diabetes Vs diabetes with Obesity seems to double.
Fatty Liver ( Steatosis)
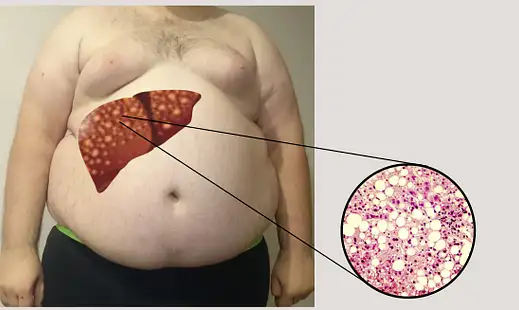
There is hardly anyone who does not know about fatty Liver, that’s because it’s very common and routinely found on an abdominal ultrasound examination. The cause of fatty
Liver can be broadly divided into two categories: alcoholic and nonalcoholic.
It’s true – while Obesity and alcoholism are two very different health issues, they can impact the Liver in the same way, i.e. causing fatty deposits in the Liver – a condition called fatty liver disease. Compared to heavy drinkers, it is now seen that non-drinkers are frequently seen to have fatty Liver, especially among obese or have Type 2 diabetes. Fatty Liver in this category is termed NAFLD (Non-Alcoholic Fatty Liver Disease).
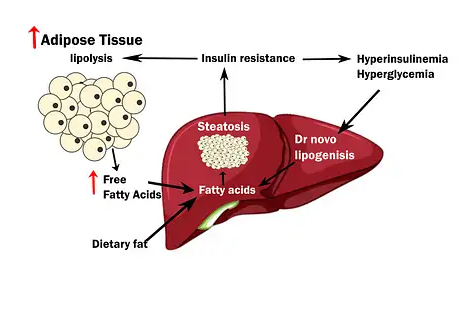
NAFLD, which covers a major percentage of liver disease, needs to be understood in detail because in later stages, as it progresses, it can lead to cirrhosis and liver failure and liver cancer. The Obesity is associated with an increased risk of nonalcoholic fatty liver disease (NAFLD). Steatosis, the hallmark feature of NAFLD, occurs when hepatic fatty acid uptake from plasma and de novo fatty acid synthesis is greater than the rate of fatty acid oxidation and export (as triglyceride within VLDL). Therefore, an excessive amount of intrahepatic triglyceride represents an imbalance between complex interactions of metabolic events.
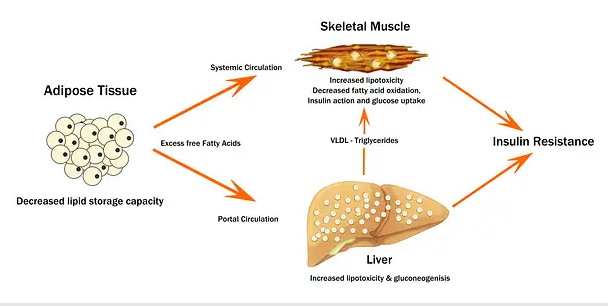
The presence of steatosis is associated with a constellation of adverse alterations in glucose, fatty acid and lipoprotein metabolism. It is likely that abnormalities in fatty acid metabolism, in conjunction with adipose tissue, hepatic, and systemic inflammation, are key factors involved in the development of insulin resistance, dyslipidemia and other cardiometabolic risk factors associated with NAFLD. However, it is not clear whether NAFLD causes metabolic dysfunction or whether metabolic dysfunction is responsible for IHTG accumulation, or possibly both. Understanding the precise factors involved in the pathogenesis and pathophysiology of NAFLD will provide important insights into the mechanisms responsible for the cardiometabolic complications of Obesity.
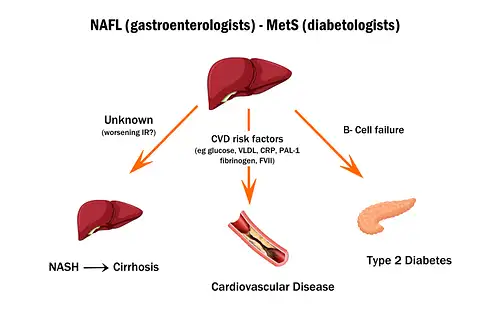
The association of NAFLD with serious cardiometabolic abnormalities, including type 2 diabetes mellitus (T2DM), the metabolic syndrome and coronary heart disease (CHD).
The hallmark feature of NAFLD is steatosis i.e excessive intrahepatic triglyceride (IHTG), approximately when 5% or more of hepatocytes contain visible intracellular triglycerides.
IHTG can be evaluated by using magnetic resonance spectroscopy (MRS).
Steatosis develops when the rate of FA input (uptake and synthesis with subsequent esterification to TG) is greater than the rate of FA output (oxidation and secretion).
Therefore, the amount of TG present in hepatocytes represents a complex interaction among 1) hepatic fatty acid uptake, derived from plasma free fatty acid (FFA) released from hydrolysis of adipose tissue TG and FFA released from hydrolysis of circulating TG,
2) de novo fatty acid synthesis (de novo lipogenesis )
3) fatty acid oxidation (FAO), and
4) fatty acid export within VLDL-TG.
A central abnormality in the pathogenesis of steatosis appears to be insulin resistance resulting in lipolysis, which increases circulating free fatty acids, which are then taken up by the Liver as an energy source. The fatty acids overload the hepatic mitochondrial β-oxidation system, leading to the accumulation of fatty acids in the Liver. Indeed, some investigators suggest NAFLD be the hepatic manifestation of insulin resistance syndrome.
NAFLD does not universally progress to NASH, and the precise pathogenesis of steatohepatitis is yet to be determined.
Adipokines, tumour necrosis factor (TNF)-α and adiponectin play a role in lipolysis.
TNF-α, which interferes with insulin signalling, thereby favouring steatosis, and also TNF-α is also proinflammatory and, thus, may play a role in the pathogenesis of the inflammation in NASH.
Adiponectin is antilipogenic and anti-inflammatory. Adiponectin levels are decreased in conditions associated with NAFLD, including insulin resistance, Obesity, type 2 diabetes, and NAFLD.
Adiponectin and TNF-α, therefore, have opposing effects. The net result of increased TNF-α and decreased adiponectin is prosteatotic and proinflammatory.
Fatty acids in the Liver induce the formation of free radicals, which cause lipid peroxidation and induce proinflammatory cytokines. This results in the formation of Mallory’s hyaline in the hepatocyte and activation of the stellate cells, which leads to collagen synthesis and fibrosis—the three characteristic histologic features of NASH.
NASH has been linked to an increased risk of heart attack and stroke
A liver affected by NASH may produce inflammatory factors that promote the atherosclerotic process that narrows blood vesselsThe cause of NASH, not NASH itself, may increase heart attack and stroke risk. NASH is frequently associated with Obesity, especially visceral fat, and is intimately related to fatty liver and insulin resistance syndrome markers. Identifying obese patients who may progress from steatosis to NASH and from NASH to fibrosis/cirrhosis is a significant clinical challenge.
CIRRHOSIS and Liver failure
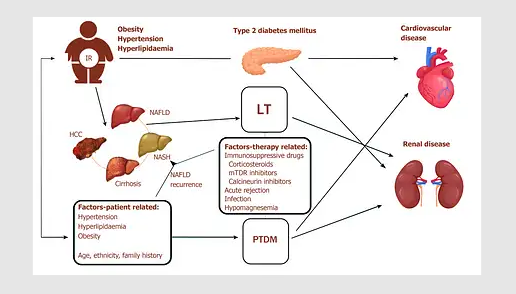
The progression from NASH to cirrhosis is seen rapidly if Obesity is associated with type 2 diabetes. The major cause of cryptogenic cirrhosis is type 2 diabetes. Also, the association between diabetes with hepatitis C is high, so much so that it is better and safer to screen patients with type 2 diabetes and persistently elevated serum ALT for HCV.
In fact, the entire spectrum of liver disease from abnormal liver enzymes, nonalcoholic fatty liver disease (NAFLD), cirrhosis, hepatocellular carcinoma, and acute liver failure is seen in type 2 diabetes. The risk of acute on chronic liver failure s high in morbidly obese patients and this could be attributed to the chronic inflammatory state associated with morbid Obesity.
Acute liver failure
The incidence of acute liver failure appears to be increased in patients with diabetes: It remains unclear whether it is diabetes, medications, or other factors that account for the increased risk of acute liver failure. Troglitazone was factored out in these studies.
Investigating a patient with liver disease, Liver function tests
1. Hepatitis C (anti-HCV or HCV PCR),
2. Hepatitis B (HBV surface antigen),
3. Hemochromatosis (iron and iron saturation),
4. HBA1C
5. Abdominal ultrasound.
6. Patients with hepatitis C, hepatitis B, and increased iron saturation need a referral for further workup and treatment.
7. Ultrasound has a positive predictive value of 96% for detecting NAFLD in the absence of other liver diseases
8. Magnetic resonance spectroscopy (MRS)
9. Hepatic Fibroscan
10. Upper GI endoscopy
11. CT Abdomen
Management of NAFLD
1) Lifestyle intervention plays a significant role in the remission of NAFLD in patients with Obesity and without Obesity. It’s as simple as that. You need to know and take appropriate steps. If one is obese or diabetic, have a medical checkup done, get investigated before you are caught by surprise. A calorie restriction leading to even 5 to 10% weight loss can lead to a marked decrease in IHTG content and improved hepatic and skeletal muscle insulin sensitivity, improvement in liver biochemistries, liver histology (steatosis and inflammation).
2) Bariatric surgery is the most effective available weight loss therapy in those who are non-responding to medical methods / non-surgical procedures of weight loss. There has been concern that the significant and rapid weight loss induced by bariatric surgery can worsen NAFLD by increasing hepatic inflammation and fibrosis. However, data from more recent surgical series suggest that weight loss induced by bariatric surgery decreases steatosis, inflammation and fibrosis.
Also, bariatric surgery-induced weight loss has considerable beneficial metabolic effects in the Liver manifested by a decrease in:
1. Hepatic glucose production.
2. Hepatic VLDL-triglyceride secretion rate.
3. Hepatic gene expression of factors that regulate hepatic inflammation and fibrogenesis.
These data suggest that bariatric surgery-induced weight loss is an effective therapy for NAFLD in patients with morbid Obesity by normalizing the metabolic abnormalities involved in the pathogenesis and pathophysiology of NAFLD and preventing the progression of hepatic inflammation and fibrosis.
3) If a simple bariatric surgery is added to a liver transplant surgery in a morbidly obese person, the liver transplant results could be much better. However, the feasibility of the operative time and how the patient is withstanding the transplant procedure will be the primary deciding factor.